Photo and article by Mary Alice Murphy
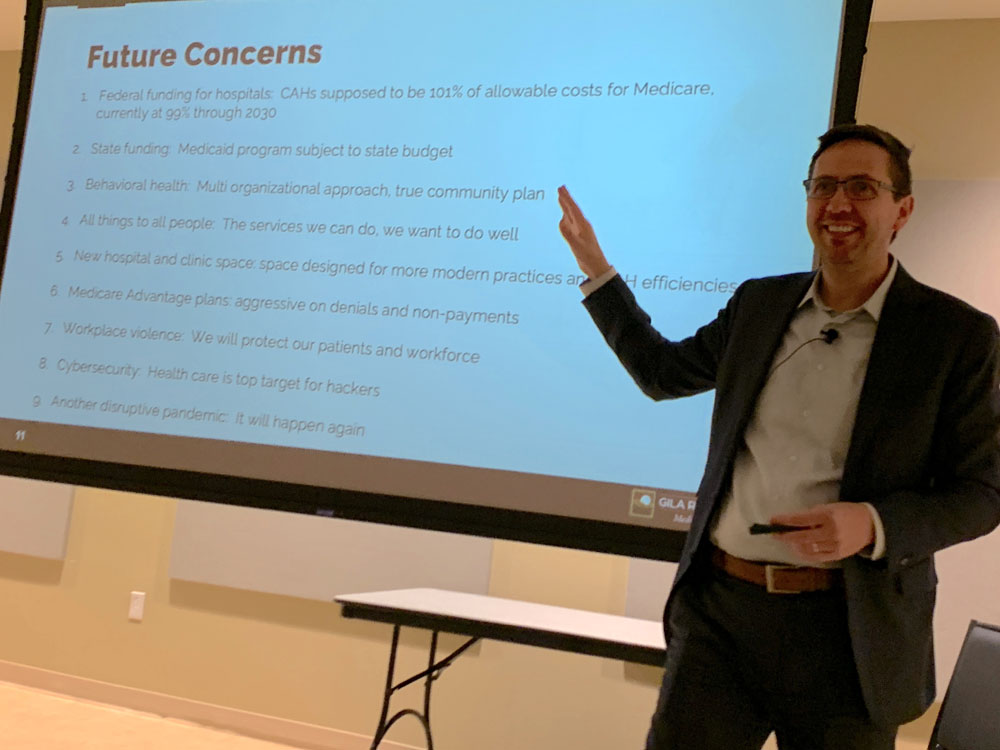 GRMC CEO Robert Whitaker led a townhall for about 70 people and talked about the hospital and in this photo about his future concerns.
GRMC CEO Robert Whitaker led a townhall for about 70 people and talked about the hospital and in this photo about his future concerns.
Gila Regional Medical Center Chief Executive Officer Robert Whitaker opened the townhall at the Grant County Veterans Memorial Business and Conference Center on Jan. 10, 2024, by introducing himself as the new permanent CEO for the hospital.
He said he would talk about what is happening at the hospital, and he looked forward to answering questions at the end. "Pay attention, because there will be a test at the end," he chuckled.
"My family is here," he said. "I'm originally from Houston, born and raised there. Actually I lived a few years overseas where my father was a petrochemical engineer. We lived in Indonesia and Algeria, seven years combined. I have an industrial engineering degree from the University of Houston. I picked industrial out of all the engineering degrees because it required the least amount of chemistry. I do have a master's in public health and that's what drove me into hospital management. I also have extended family living in New Mexico."
His first career was in the petroleum industry, as a pipe fitter and boilermaker. "I married the right gal and went to college. My father-in-law was the director of facilities at a large hospital and he gave us a tour. While we we walking, I said these exact words: 'I never want to work in an hospital.' In college I wanted to build large plants and refineries, but my first job was managing large construction projects at a hospital. That's what guided me into hospital administration. I started out in hospital finance, then did some operations stuff. I worked at a large for-profit hospital system. They moved me around into non-profit and government hospitals as well."
He then recognized some folks among the people attending the townhall. He said the chief financial officer at that time was Leonard Brinkley, but "we have a new one, a permanent CFO William Ermann coming in on Jan. 22."
He also recognized some of the other administrative team members and some of the Board of Trustees. who attended, as well as GRMC medical staff. "I look at our medical staff as partners. We have a fantastic group here. Last, but not least, I want to thank our county commissioners, who, up until this last June, served as the governing board of the hospital. They made a lot of good decisions, a lot of tough decisions that brought us to where we are today."
Whitaker talked about certifications, recognitions and the like. "There is a whole host of agencies that have an impact on us and what we do, including CMS (Centers for Medicare and Medicaid), who accredit us through the Joint Commission with a comprehensive survey and visits."
He noted that Gila Regional has a Level 4 Trauma Center designation, which is accredited through the New Mexico Department of Health.
The hospital also has an accredited Rural Health Clinic. He also mentioned the accredited HeartFlow system, which helps the cardiologist determine the needs of heart patients.
The next things on the list for accreditation include becoming an accredited stroke center, a heart center and an orthopedic center.
"Of the 450 employees we have some are PRN, which means they work on demand, perhaps one or two days a week," Whitaker said. "Our last fiscal year we had $34 million in salaries, wages and benefits. That's a big contribution to our community and Grant County. We have 178 medical staff members. The number I really appreciate is that they represent 23 different medical specialities. That's a good variety."
He then rhetorically asked: "How busy are we? Some places count you when you come in; others count you when you leave. We count you when you leave as discharges. Over the past year, we've had about 1300 admissions, including about 3,000 surgeries ( some outpatient), 300 births and our emergency room sees about 17,000 a year. That's a busy ER. Our outpatient volumes, which we call patient encounters, are about 60,000 a year and our cancer center saw about 4,900 last year, and we'll probably go above that this year."
"This place is amazing in what it does," Whitaker said. "The cancer center offers 3D radiology, where the machine can see a cancer cell and shape the radiation beam to match the cancer cell as a specific target. We have medical oncology, which is the drugs and chemotherapy treatments.
"Another fantastic thing we have that is amazing is our outpatients with the size of our community and what we offer," he continued. He listed some of the services: lymphedema, vestibular, such as dizziness, dysphasia with swallowing issues. "We also have three pools, two of which are in active use for aquatherapy."
"All of this translates to how our hospital is doing financially," Whitaker said. "From 2013-2020, the hospital lost $48 million in operating costs. From 2021-2023, we had a net surplus of almost $34 million. Good turn around. Charity care and bad debt in 2023 totaled just over $5 million. That's a good contribution to the community."
He talked about the balance sheet, talking about days of cash on hand, "which means if you didn't have another dollar of revenue come in, how many days could you meet all of your expenses? In March 2020, GRMC had 9 days of cash on hand. In December 2023, we had 140 days of cash on hand. In the past few years, we made capital investments in the amount of $8.3 million. At the last board meeting, we were sitting on just under $34 million in cash. Those are good numbers, though we still have a ways to go, They are from our audited financials, which are audited each year. If anyone says the hospital is losing money or it's in the hole, it's just not true."
Whitaker explained that GRMC is managed by a health management company called Health Tech brought on by the commissioners, when they were serving as the board. They brought it on to create stability and viability for the long term and to make sure that patients want to come to the facility and people want to work there.Health Tech provides financial oversight and accountability for the administration, "making sure we're doing things that are best for Gila Regional. They also provide services like a group purchasing organization, which gives us discounts. In full transparency, I am employed by the management company. I've heard the question, where do your loyalties lie?"
"I'm here to make sure that everything is done for the best for the hospital and the community. There are no separate loyalties. I'm here for stability of leadership."
A man asked how long Health Tech has been at Gila Regional and what is the annual fee.
Whitaker said Health Tech came to GRMC in May 2020. The fee is in the contract. "I can't disclose the management fee, but it is a small amount. It's not an exorbitant amount."
A woman in the audience noted it was a high level of accountability for the administration.
Whitaker agreed and said every two weeks they hold a management call and every two weeks a financial call. "They also have a clinical officer who makes sure we're doing things correctly. She'll come back to work with staff on a mock survey for accreditation, so they can always be ready for a Joint Commission survey."
A woman asked him to talk about the fact that no tax dollars are levied for the hospital.
"Thank you. I underlined it and didn't mention it," Whitaker said. "Gila Regional is a county-owned facility and our audit goes out along with the county's audit. Our board of trustees members are appointed by the County Commission. Some places may have a mil levy that the residents of the county will vote on to help support the facility. Here, there are no local taxpayer funds going to support operations, infrastructure or the like. We do get capital outlay funding from the state and state, and federal grants, but no taxes that anyone pays specifically to support us. With the help of Health Tech, we've looked for other funding sources. There are people out there who do want to help hospitals, especially rural hospitals, with their capital improvements. With an MRI, it costs about a million and a half dollars to replace it. We do about 20 CT scans a day, almost one an hour every day. We are looking at replacing the MRI and the CT. We have submitted to the state for the CT, and to the federal government for the MRI."
He noted the baseline beds cost about $12,000-$13,000 each, and the ICU beds about $20,000 each, so it's a considerable expense. A fully-equipped EMS vehicle is about $324,000, and a couple of the ambulances have more the 400,000 miles on them.
"The labor and delivery unit renovation is starting Monday, " Whitaker said. "Capital needs for the hospital are not cheap. In the OR, we have six operating rooms, two are a bit larger for the orthopedic surgeries. To change out the air-handling control system, it will cost $1.3 million to change out two rooms. We got an EDA grant to fund it. We finally have some funding to put into facility and equipment improvements, but we still have more to do."
He talked about the courtyard in the middle of the hospital."We had to close it because roots were pushing up the concrete and we had a couple of people trip on them. In the spring we 'll do renovations. We need to renovate the registration area for surgeries. We're going on to over 40 years for this hospital. The way we function now as a critical access hospital and the way we treat nowadays has changed. A lot is outpatient, which is a good thing. We have a lot of inefficiencies in the hospital, such as that's it's costing us $2 million just for the labor and delivery renovation."
Whitaker continued: "Next are my future concerns in the back of my mind. One is government funding. As a critical access hospital, Medicare reimburses us by law at 101 percent of our viable cost. There was a budget bill passed in 2011 that reduced that to 99 percent, making it difficult to have a balanced budget. There are discussions about cutting that down to 98 percent, but there's been no discussion about what will happen after 2023, whether they are going to push it out longer or cut it down. Another concern I have is state funding for Medicaid. And that depends on the state budget. We have a big chart of what we can do for a patient on Medicaid and be reimbursed. We're plus in every category at 120 percent, 140 percent, but that's all because we have funds in the budget. It's a concern if state funds get tight again."
On the issue of behavioral health, he said: "We hear: 'are you ever going to open the behavioral health unit (BHU)?' The answer is: 'No.' In regards to inpatient behavioral health, there simply are not enough providers to run a program here or any other small hospital. We can't sustain the costs without 24/7 providers and care. I can say that behavioral health is important to our county government. I have talked to the state, and they would like to develop some sort of regional behavioral health system. On the outpatient side, we have a community plan, which includes law enforcement and schools and us and all the independent practitioners and provider groups. It's more than inpatient behavioral health. The city of Farmington gave a great presentation, and I know we have had some follow-up conversation. I can't be UNM. We don't have the size or population to be all things to all people. That's hard to say. What we do want to focus on are the things we can do, such as the ER, surgeries, MRIs, CTs. The things we can do, we want to do very well. That's important. "
Whitaker said the 40-plus-year-old facility, which has become a critical access hospital, allowing the use of 25 beds at any time, instead of the originally planned 62 beds, "gives us space to do things differently, such as clinics."
He noted that the Medicare Advantage, is what Medicare is pushing people to. "I'm not necessarily opposed to it, but it doesn't benefit the hospital. I was on a call with other hospital administrators and one hospital had a large percentage of Medicare Advantage patients, and 20 percent of the claims were denied. With traditional Medicare, it's about 4 percent being denied. We all need insurance, but they are aggressive with denials and non--payments. It's a concern, so we have to counteract that by putting our resources toward it. We have to spend more to make sure we're bringing in the money that we should."
Workplace violence is another concern, and he said it's likely connected to behavioral health. He cited a shooting in a hospital in Dallas a couple of months ago. "The sad reality is that it's going to get worse, so we have to do things to protect our patients and our staff. It's important to us. It's so important to me that I created a new Safety Patient and Workforce Committee. It is looking at new protocols and policies."
Cybersecurity is another big concern. "Health care facilities are the top target for hackers. Why is that? It's because health care information is protected by federal law. If that gets put out to the public, there are serious fines and penalties that can come down. Hackers know this, so they hack in and then say: 'I've got your stuff. Either you pay me a million dollars or I'm going to put it out publicly and you get fined $5 million. Which do you prefer?'"
"Most hospitals are very aggressive in protecting patient information," Whitaker said. "But a lot of the data is accessible to third-party contractors. We have stipulations in place that say if this information gets out, you are liable. But that's just paper contracts. Lovelace recently got hacked and their entire system went down. Big hospitals, small hospitals, it doesn't matter, these guys are looking for a way in and a payday."
He noted that Covid-19 was disruptive. "There will be something else. There was an Ebola scare. Now that we've been through this, if there is another pandemic, we will go back to the same protocols, and it will be disruptive again, including challenges on supplies and being able to care for patients. Hospitals were full, and if you needed to transfer a patient, those hospitals were full, too."
A participant asked how far behind had denials put the hospital. White replied that he didn't have the numbers, he was just putting out the concern with the process. The government payers' denials are greater than from the private insurance providers.
A woman asked about the possibility of a regional behavioral health facility.
"That's the discussion," Whitaker said. "The New Mexico Hospital Association includes all the hospitals in the state. There's also a New Mexico Rural Hospital Association with 11 members. We are part of both. We've talked about this, and Las Cruces is probably the only location for such a facility in the southern part of the state."
He then noted that GRMC has a Level 4 Trauma Center. "We don't treat gunshots or multiple stabbings. This designation means we have staff trained in trauma. We have partnerships with other facilities that will accept those more extreme cases. We have policies and protocols. We have staff training to react. The state monitors our charts. We have Bertie Berry. To show you how well recognized our facility is, Bertie is the chair for the state Trauma Performance Improvement group. That's a great recognition for us."
"We have a YouTube channel, with two videos on it," Whitaker said. He played the one featuring Berry and EMS Director Eloy Medina explainingthat a Level 4 Trauma Center can provide stabilizing care that enhances the chance of full recovery for the patient, including 24/7 emergency care and diagnostic services to allow a patient to be safely transported for more comprehensive care when needed.
He then answered the question: What is a critical access hospital?
"I've heard that people think it means the hospital will have to cut back on services," Whitaker said. "That is not true. There are only two limiting factors. The first is that we can have no more than 25 inpatients at any time. When we look at year-to-date numbers, we're at about 11.1, so there's no concern for us to worry about not having enough room to take care of our patients. Some days it goes up to maybe 18 to 19. ER holds don't count into the number nor do births. The only other limiting factor is our average length of stay. We record it for every patient and the average stay has to be four days or less. Some stays are longer up to seven or eight days to care for our patients. It's the average that matters. It does not mean that after a person is there for four days we transfer them out. No, that doesn't happen. Technically, we cannot transfer someone on the same level of care to another hospital. We can transfer up if a person's condition deteriorates, for example."
Another way critical access hospitals are different is that it changes the way "we get reimbursed by Medicare. We get reimbursed on allowable and reasonable costs. There are two types of hospitals—PPS, prospective payment hospitals and critical access hospitals. On the inpatient side, PPS hospitals, and we get paid this way, too, by private insurance, we get paid by a DRG (diagnosis-related group). Our federal government Medicare in its infinite wisdom has created a numeric number for everything a hospital could ever do to a human being clinically. Say a person comes into a PPS hospital with pneumonia. The DRG says that's No. 500—I'm making all these numbers up—and payment is $5,000, no matter how long a stay or how many drugs or how much care or how many physicians, you are paid that set fee. That system works for a large hospital with large numbers of patients. For a small hospital with 11 patients that system does not work. So Medicare for critical access facilities does it by allowable and reasonable costs. Take the nursing care, Medicare allows 100 percent of that cost. How about housekeeping and office space. Then Medicare says it will allow a PPS hospital 75 percent of environmental services (housekeeping) or 50 percent of dietary. It's complicated. It benefits us as a critical access hospital, because these costs are allowable and reasonable. That's part of the history of how we got back from the loss of $44 million by being able to get reimbursed for our costs."
He said critical access has been "critical" to the hospital. Whitaker also noted that critical access hospitals can have so-called swing beds, which is skilled nursing care. "We can offer skilled nursing care to every bed. For instance, say a person with a hip replacement needs five or six days of rehab. The three days of acute care don't change, but for the rehab the person stays in the same bed, with the same staff, but gets the rehab in a swing bed. Medicare gives you up to 100 days of skilled nursing care in a year and they will pay for it. Medicare pays 100 percent for the first 20 days, then 80 percent after that. It's a careful balance to make sure the person doesn't reach 100 days by May. Swing bed is a Medicare program."
He showed another short video, which showed the first person who received the swing bed service at Gila Regional.
A man asked about the number of days. Whitaker said the up to four days of acute care do not count toward the swing bed care number of days. "The program keeps patients from having to transfer to another facility for skilled nursing care. But if they are a resident of a nursing facility, if they need skilled nursing care they can get it there, and it counts toward that person's 100-day limit. "
"I can't emphasize enough how important the critical access hospital designation is to our small hospital to make us financially stable and sustainable," Whitaker said. "It does not limit our services."
A woman commented on a local group beginning to organize for senior care, "We help each other. I wonder if the hospital has someone specializing in stroke care for example that could help us."
Whitaker said: "We consider trauma care as important to our hospital as any of our other services. Because we do have a large population of retired people, I look at developing a geriatric service line and have someone that oversees that, like Bertie does for trauma."
He talked about community engagement. "One thing I want to do is a community health needs assessment, because it's important. It's not a Gila Regional assessment but a community needs assessment. We will partner with others and get a vendor to do it."
"We want to create a community benefit report," Whitaker said. "I've presented to several towns already. We want to talk about health and wellness, and we will talk with the schools. We need people in all trades. We need more people in health care, too. Hospitals are not just nurses, but also lab people, therapy. With workplaces and businesses, we want to make sure we provide what the businesses needs to maintain a strong, healthy workforce. We want to be a good partner with independent and group practices. There's a lot of public health initiatives, we want to help with."
He said it comes down to the hospital's four aims. "One, we want to improve patient outcomes. We want people to leave better than when they came in. Two, we want to enhance the patient experience. We know that patients are our customers. Three, we want to take care of our caregivers. We want to recruit and retain qualified, competent members of our workforce. All employees, regardless of their department are caregivers. Four, we want to reduce the cost of care. We want to be good stewards of our finances."
He then began the question and answer period.
A person asked if she could get a copy of the presentation. He said he would work on it.
A woman said he had mentioned replacing the MRI. "How's the one you have working?
Whitaker assured her that it was working fine. "We're just being proactive."
A woman asked about community engagement. "Is there a place where people can go in to talk to anyone?"
Whitaker said he isn't yet aware of all the entities, but to talk to him, just go in the front door of the hospital, turn left and the first door has his name on it to talk to him.
The same woman asked about equipment. "Is it possible to have a mil levy for just a year or something?"
"That's the last thing we want to do," Whitaker. "We don't want that to happen. We don't want to be a burden on anyone for tax dollars."
Another woman asked about the swing bed program and how many patients they had served with it so far. Whitaker replied: "Three."
A man said he would like to see one person at the hospital who was in charge of senior care, so someone could go and ask questions of that person. Whitaker said that was of interest to him ,also.
The next question was hard to hear, but she asked about radiology. Whitaker said: "We already have a linear accelerator at a cost of about $4 million, along with the calibration unit that goes with it. "
Another woman asked if a person could come back in after, say 30 days, and be eligible for a swing bed. "Great question," Whitaker said. "In order for a person to be eligible for skilled nursing care, according to Medicare, the person would have to have or have had three acute care midnights. Yes, we serve as a skilled nursing facility, and there is a small window where one can return."
A man asked another question. "When you walk around town and talk to people, do you have a PR plan for public announcements for better public information?"
"This is the start of it," Whitaker said. "We have the two videos and we will improve on that with community outreach."
A man spoke softly and Whitaker said he would get the man's information and follow up.
Another man asked about the helicopter transfers and who bears the cost. Whitaker said it's a mix of payments. Insurance pays for at least part of it. "But sometimes, it's where charity care comes in."
A man asked a question. Whitaker said he listed all of his concerns. "Every one of them has a financial aspect to it. There are rural hospitals in New Mexico that have higher days of cash than we do. How will a new hospital ever get funded? There are things we need to do to prepare ourselves for what we know is coming down the road, as well as what we don't know is coming down the road. I don't have a number that we want to reach. we want to see the number incline rather than decline."
To another comment, Whitaker said for anyone who was not aware, the hospital contracted with a physician group that provided emergency room care. "They left the state because of its high medical liability costs. There was recently a judgement on a hospital of $68 million. They chose to leave. Those costs come back on us. We have contracted with a new ER provider group from Las Cruces. It's competitive right now. We have physicians that come from Las Cruces that come when needed. We're working on getting a stable group here."
A man asked if there was one type of cardiac care that the ER sees. A woman replied there are different ones, but heart attacks are generally transferred out for more comprehensive care than can be provided at GRMC.
Another man asked about behavioral health being a big problem in the community, with the homeless and the lack of responders.
Whitaker said that question is likely being asked in all the rural towns. "Hospitals simply don't have the staff to provide the behavioral health care. Inpatients are impossible for the near future. Yes, I appreciate the regional portion. We are the only ones who can take in patients, and we can provide outpatient care, but not behavioral health inpatient care. It's not just us that are involved, but also law enforcement and schools. None of us has the capacity to take care of the needs."
He said he would stay as long as there were questions, but no one else had any, and the session ended with applause from the attendees.